It’s not just antibacterial resistance; now FUNGAL resistance labeled a huge threat to medicine
07/07/2017 / By Russel Davis
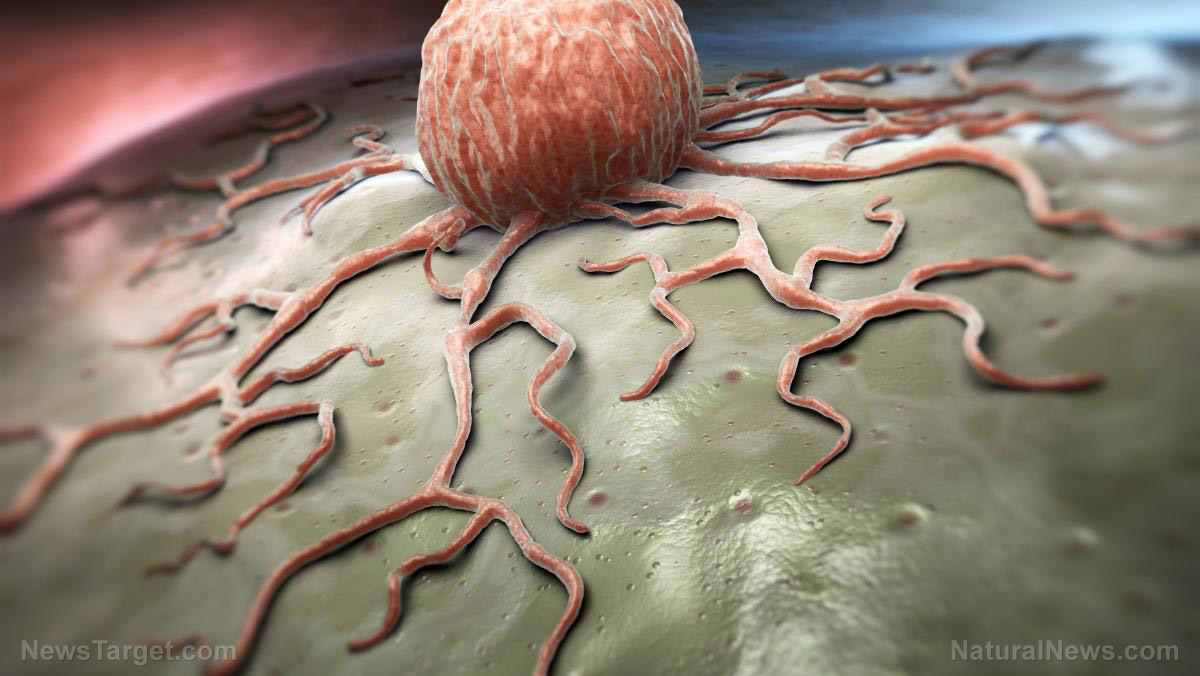
The current microbial resistance crisis has given way to yet another potential medical crisis by way of fungal drug resistance, said Ambalika Batra, a post-doctoral scientist at Royal Holloway University in London. According to Batra, patients were dying as physicians were finding it increasingly challenging to address fungal infections. According to the expert, fungal infections accounted for about 1.7 million deaths annually worldwide. This was due to some fungi species becoming more resistant to antifungal treatments.
Batra also stressed that misdiagnosis plays a role in the prevailing fungal resistance. For instance, the fatal Candida auris fungus was often misdiagnosed as the less dangerous Candida haemulonii. As a result, the misdiagnosis may have contributed to the ongoing resistance crisis. Additionally, Batra noted that the most serious fungal infections occur in hospitalized patients and individuals with compromised immunity.
Moreover, the health expert emphasized that the lack of quick and accurate diagnosis further exacerbated fungal resistance. Batra said the absence of an accurate diagnostic test often led to the prescription of broad-acting antimicrobial drugs that do not distinguish good microbes from the bad ones. In turn, this lack of accurate diagnosis not only caused preventable deaths but also aggravated antimicrobial resistance. According to Batra, more drugs used equated to greater risk of spreading resistant bacteria and fungi across populations.
Furthermore, the health expert quipped that while faster and easier bacterial and viral diagnostic tests have already been developed, tests for fungal infections seemed to have lagged behind. According to Batra, fungal infections are still diagnosed using blood culture tests. The lengthy, 14-day process involved incubating a patient’s blood sample and waiting until the fungus grew enough to be detected. Only then could specially-trained microbiologists step in to identify the type of fungi that infected the patient.
100% organic essential oil sets now available for your home and personal care, including Rosemary, Oregano, Eucalyptus, Tea Tree, Clary Sage and more, all 100% organic and laboratory tested for safety. A multitude of uses, from stress reduction to topical first aid. See the complete listing here, and help support this news site.
According to Global Action Fund for Fungal Infections, more than 80 percent of patients could be spared from the infection if specialized tests and antifungals were available everywhere, and were wisely utilized by physicians. However, Batra noted that molecular diagnostic tests may serve as a good alternative. Molecular diagnostic tests only needs to detect DNA of small amounts of fungus. This means that a smaller blood sample is needed, and that the infection can be detected earlier.
CDC recognizes growing concern; offers a few tips
The Centers for Disease Control and Prevention (CDC) acknowledged that antifungal resistance has become a growing concern in the medical field. The CDC noted that the fungus Candida appeared to have developed resistance against the first-line and second-line antifungal medications fluconazole and echinocandins, respectively. According to the federal agency, resistance to fluconazole remained stable over the past 20 years. However, resistance to echinocandins has been showing an upward trend. Aside from Candida, the fungus Aspergillus has also exhibited some form of resistance over the years. However, the federal agency quipped that the extent of this resistance remains unclear. (Related: Herbs and diet to kill Candida and other fungal, yeast infections)
In line with the growing concern over fungal resistance, the CDC has offered a few tips to reduce resistance:
1. For hospital executives and infection control staff
- Evaluate antifungal use as part of antibiotic stewardship initiatives.
- Ensure that guidelines on proper hand hygiene and infection prevention are being met.
2. For physicians and other hospital personnel
- Prescribe antifungal drugs appropriately.
- Record the dose, frequency, and indication for each prescription.
- Monitor local antifungal resistance patterns.
- Join and lead hospital initiatives that improve antifungal prescribing practices.
- Follow proper hand hygiene and infection control standards with each patient.
3. For hospital patients
- Ensure that everyone sanitizes their hands before entering your room.
- Inquire if catheter use is necessary.
Sources include:
Tagged Under: antibacterial resistance, fungal infection, fungal resistance, infection, infections, microbial resistance, superbugs