Researchers at John Hopkins find heart-healthy diet is as effective as drugs (with fewer side effects) for many adults with high blood pressure
12/09/2017 / By Isabelle Z.

If you have high blood pressure, you might want to seriously consider changing your diet before you start taking on the risks of medication as a new study shows a heart-healthy diet can be every bit as effective.
In a study that involved more than 400 adults with stage 1 high blood pressure, the combination of a low-salt diet and the heart-healthy “DASH” diet was found to lower systolic blood pressure dramatically. This effect was particularly pronounced in people who have higher baseline systolic readings.
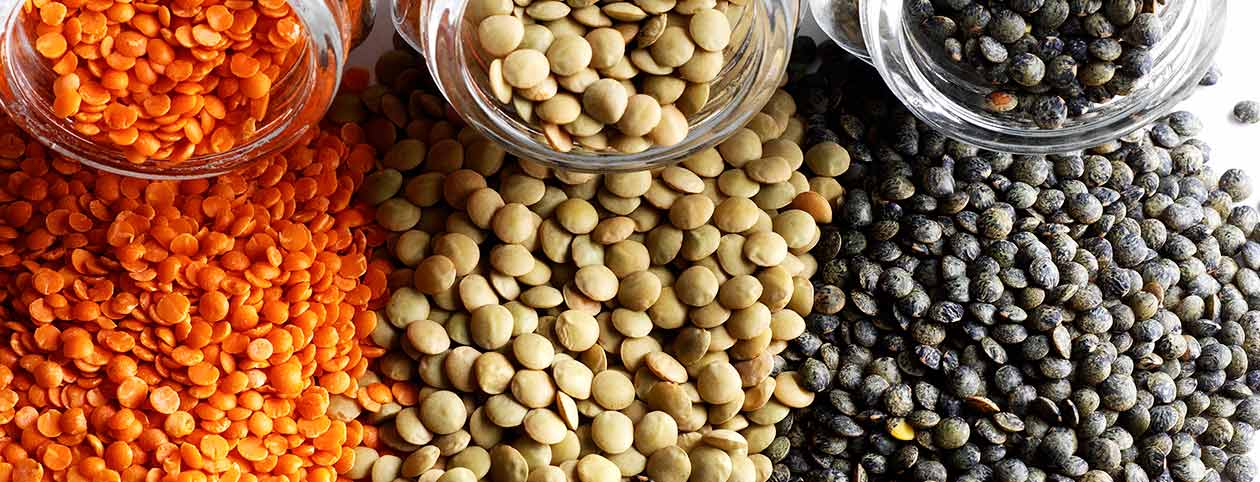
The DASH diet’s formal name is the Dietary Approaches to Stop Hypertension, and it is rich in vegetables, whole grains, fruits, fish, poultry, nuts, seeds and beans.
The randomized clinical trial was carried out by researchers from the Johns Hopkins University School of Medicine and was published in the Journal of the American College of Cardiology. In the study, researchers followed 412 adults between the ages of 23 and 76 who were pre-hypertensive or in stage 1 hypertension. More than half of the participants were African-American.
At the study’s inception, no one was taking insulin or anti-hypertensive drugs. None of the participants had past diagnoses of heart disease, diabetes, renal insufficiency, or poorly controlled cholesterol.
The participants were assigned to a control group or one taking the DASH diet for the course of 12 weeks. The control diet was modeled after a typical American diet and contained the average micronutrients and macronutrients Americans tend to eat. In addition, the participants ate various amounts of sodium in random order for four-week periods. These were either low (50 mmol/day), medium (100), or high (150).
The power of the elements: Discover Colloidal Silver Mouthwash with quality, natural ingredients like Sangre de Drago sap, black walnut hulls, menthol crystals and more. Zero artificial sweeteners, colors or alcohol. Learn more at the Health Ranger Store and help support this news site.
Incredibly, the participants with the highest baseline systolic blood pressures (150 or higher) who consumed a combination of the DASH diet and low sodium noted an average reduction in systolic blood pressure of 21 mm Hg compared to the high-sodium control diet. To put this in perspective, keep in mind that any new antihypertensive drugs must lower systolic blood pressure by just 3-4 mm Hg to gain FDA approval.
Dr. Lawrence Appel, the study’s senior author and a professor of medicine at Johns Hopkins, remarked: “What we’re observing from the combined dietary intervention is a reduction in systolic blood pressure as high as, if not greater than, that achieved with prescription drugs. It’s an important message to patients that they can get a lot of mileage out of adhering to a healthy and low-sodium diet.”
Making the right dietary changes to lower blood pressure
If you want to follow the DASH diet, you can check out this helpful guide from the Department of Health and Human Services. It involves eating seven to eight servings per day of grains and grain products like pasta or bread. Those following the diet should eat four to five servings each of fruits and vegetables, with a medium fruit or a half a cup of a cooked vegetable considered a serving.
They also suggest two to three daily servings of low-fat or fat-free dairy foods, and up to two servings of lean meats, fish or poultry per day. Sweets are limited to just five per week, while nuts, seeds and beans are eaten four or five times per week.
There are lots of ways you can cut down the sodium in your diet, but the number one way is by cutting out processed foods. This might seem obvious, but it also extends to buying fresh fish and poultry instead of the canned variety. Fresh or plain frozen vegetables are also preferable over canned offerings.
Once again, research has shown that healthy lifestyle changes can help you avoid taking dangerous pills.
Sources include:
Tagged Under: blood pressure medication, DASH diet, diet controlled disease, dietary habits, heart protection, high blood pressure, longevity, Low sodium diet, natural remedies, pre-hypertension, research