The brain-gut connection: A new study finds that traumatic brain injury also causes intestinal damage
12/22/2017 / By Ralph Flores
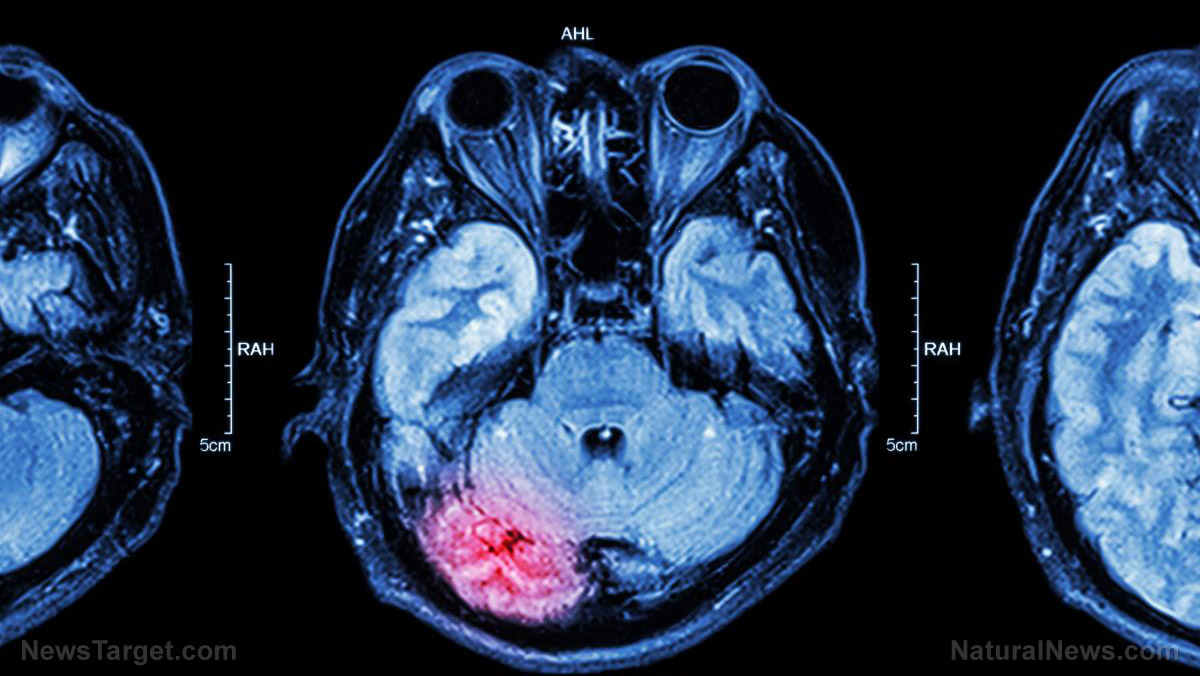
Traumatic brain injury (TBI), aside from causing damage to the brain, can also damage a person’s gut, according to a study published by the University of Maryland School of Medicine (UMSOM). Then, in what can only be a described as a vicious cycle — the damage that he receives in the gut may likely cause more damage to his brain. This disturbing pattern is responsible for the upswing in reported cases of infection and chronic brain damage of patients.
Previous studies have already noted a connection between TBI and gastrointestinal dysfunction, stating that TBI affects intestinal permeability (the ability of the gut to allow materials from the intestine into the bloodstream). However, the study, which was published in the journal Brain, Behavior, and Immunity, was the first to correlate TBI in mice with “delayed, long-term changes in the colon” and link it back to post-traumatic brain inflammation and associated tissue loss.
Through in vivo studies, researchers were able to determine that mice which sustained TBI had an increase in permeability (the attribute of an object to pass through) in their gut a month after the injury. This increased permeability means that the colon allows more objects to pass through it and enter the bloodstream. Researchers posited that harmful microbes might be allowed to move into different areas of the body with this condition — which could ultimately lead to infection. This could help explain the rise in mortality rates of people who have TBI, who are 12 times more likely to die from bacteria-related blood poisoning and 2.5 times more likely to die from a problem in the digestive system. (Related: Homeopathic Medicines for Traumatic Head Injury)
Mother Nature's micronutrient secret: Organic Broccoli Sprout Capsules now available, delivering 280mg of high-density nutrition, including the extraordinary "sulforaphane" and "glucosinolate" nutrients found only in cruciferous healing foods. Every lot laboratory tested. See availability here.
The direct link between TBI and its effect on the intestine is still unclear; however, researchers attribute this condition to enteric glial cells (EGCs), a type of cell that is found in the gut. These cells bear a similarity to brain astroglial cells, and both cells are triggered by TBI. Experts believe the activation of the cells is a factor in brain inflammation and its delayed tissue damage.
Moreover, the study also focused on the two-way interaction of this process — how irregularities in the gut can impact the inflammation of the brain after TBI. To test this theory, the researchers infected mice with Citrobacter rodentium, a bacteria that has similar properties to Escherichia coli (E. coli) which affects humans. Results noted that mice who had TBI, when they were infected with the bacteria, had aggravated their brain inflammation over those who had no injury.
According to lead researcher Dr. Alan Faden of the UMSOM Shock, Trauma, and Anesthesiology Research Center, “These results indicate strong two-way interactions between the brain and the gut that may help explain the increased incidence of systemic infections after brain trauma and allow new treatment approaches.”
Prevention is always better than cure
TBI has far-reaching physical and psychological effects. Situations that can cause this injury include:
- Falls — These are the most common cause of TBI for older adults and young children. Falls can happen anywhere — tumbling out of bed, slipping in the bath, even falling from a flight of stairs.
- Vehicle-related collisions — Aside from causing 32,000 deaths each year, collisions involving cars, motorcycles, bicycles, and pedestrians are a common cause of TBI.
- Violence — This contributes to at least 20 percent of traumatic brain injury cases.
- Sports injuries — A number of high-impact or extreme sports can contribute to TBI cases, especially among the youth.
- Explosive blasts and combat injuries — This is a rare incident for people who are not in the military, but active-duty military personnel are highly likely to receive TBI due to explosions.
Identifying where TBI happens is the first step in making sure that it doesn’t happen to you and your family. Here are some ways to reduce your risk of a traumatic brain injury:
- Always wear a seatbelt when in a car, or any motor vehicle.
- Don’t drive if you’re under the influence of alcohol or drugs.
- Wear a helmet while riding a motorcycle or a skateboard and when playing sports.
- Check your house to identify risks.
Sources include:
Tagged Under: Brain, enteric glial cells, gut, injury, mental health, TBI, trauma, traumatic brain injury