Humans are embracing the rise of the “robosurgeon” but new studies suggest they are NOT better than human surgeons
01/05/2018 / By Jhoanna Robinson

Robotic surgeons are taking the National Health Service (NHS) by storm. They are now being used to conduct surgical operations for prostate cancer or for kidney and bladder problems, which decades ago have been the domain of human surgeons.
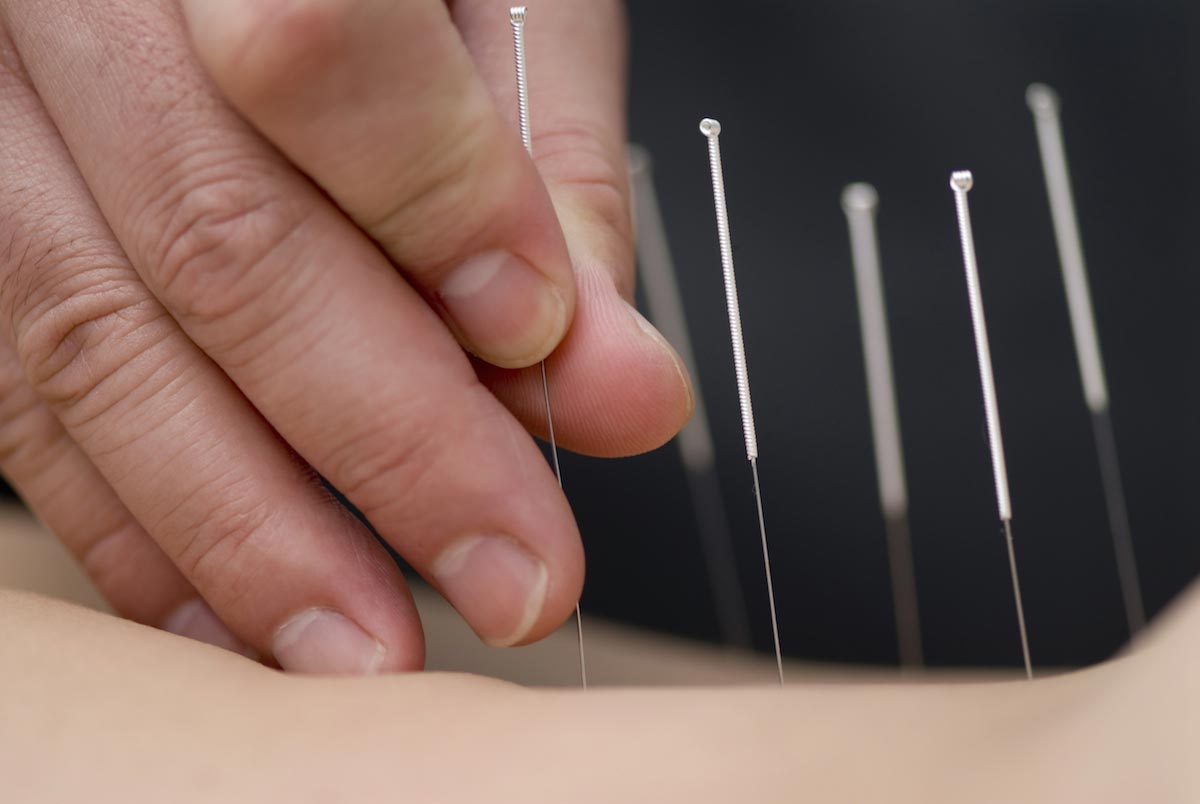
The machines, employing pinpoint-accurate, computer-controlled arms, are being hyped as devices that can be utilized to do minute surgical tasks such as cutting and stitching far more effectively than frail-fingered humans, and with no risks of bleeding from excessive incisions or poor suturing.
There are now around 60 “da Vinci” type robots in NHS hospitals. They came from the da Vinci Surgical System, a device that scales down a surgeon’s hand movements to copy the method of making tiny incisions, leading to less tissue damage and shorter recovery time for patients. They are used to get a 3D computer visual to see inside patients, or to operate tiny cameras and minuscule tools to perform procedures.
At present, almost 2,000 da Vincis have been made worldwide, and they are utilized in around 200,000 operations annually.
But do these robots live up to their expectations? After all, they are priced at around 1.7 million British pounds each and annual maintenance costs of 140,000 British pounds , according to a report by the Royal College of Surgeons Bulletin.
Studies showed that they aren’t that much better than real doctors. Clinical trial results from a study that was conducted in October 2017 by the Cochrane Library showed that even with prostate cancer operations – the most popular application for robot surgeons in the United Kingdom – the machines gained no better outcomes than keyhole surgery performed by humans.
Sponsored solution from CWC Labs: This heavy metals test kit allows you to test almost anything for 20+ heavy metals and nutritive minerals, including lead, mercury, arsenic, cadmium, aluminum and more. You can test your own hair, vitamins, well water, garden soil, superfoods, pet hair, beverages and other samples (no blood or urine). ISO accredited laboratory using ICP-MS (mass spec) analysis with parts per billion sensitivity. Learn more here.
Undergoing robot surgery would not necessarily make one less susceptible to post-surgical bleeding or operations having to be redone. As a matter of fact, keyhole operations that were done by robots did not fare better than the far more invasive, non-keyhole form of operation for prostate cancer, called open radical prostatectomy.
It could be argued, therefore, that the NHS is actually wasting money by using vital funds to purchase these robots. “The big thing about robot surgery is it’s dramatically expensive. The NHS is forking out millions of pounds and before our study we had no idea if there was any benefit,” said David Jayne, a professor of surgery at St. James’ University Hospital in Leeds.
So why do NHS hospitals still buy them? It might be due to the fact that robots offer a sales edge, because patients are more often than not secure in their belief that robots are more superior in surgery and operation skills than their human counterparts.
“Patients were attracted to centers offering robotic surgery, and other centers adopted this technology to preserve their market share. NHS trusts appear to have bought the robots not because they are better, but because they pull in more customers,” said Ajay Aggarwal, an oncology researcher at the London School of Hygiene and Tropical Medicine.
University of Surrey professor of urology Christopher Eden has conducted prostate operations using both keyhole surgery and robots. “There are a few reports that do show robotics can have slightly better outcomes, but really you are looking at the fact that the surgeons involved are high in experience and expertise. I advise anyone considering a prostate operation to look at the surgeon’s short-term and long-term outcomes, not what kit they are using,” he said.
Eden said there are areas where using robots can be more beneficial. Such is in a relatively new technique called Retzius-sparing protastectomy, which removes the prostate from the behind the patient, as opposed to the conventional surgery which removes the prostate from the front of the patient.
Eden said the Retzius-sparing protastectomy has a three-times greater rate of success of decreasing the risk of incontinence in men – a complication that 10 percent of prostate cancer patients suffer from.
For more stories on the wonders of artificial intelligence and basic and complex robotics technologies, visit Robotics.news today.
Sources include:
Tagged Under: discoveries, future tech, invasive, inventions, keyhole operations, medical technology, NHS, NHS hospitals, post-surgical bleeding, Prostate cancer, protastectomy, robosurgery, robot surgery, robotics, robots, surgical procedures