Elderly patients who have undergone surgery are more prone to “silent” strokes, caution scientists
07/09/2020 / By Virgilio Marin
Going under the knife has its risks. For older adults, however, that risk includes having a stroke without even realizing it. In a study published in the Lancet, a team of researchers found that one out of 14 older adults who had elective, non-cardiac surgery experienced a perioperative covert stroke – that is, a “silent” stroke after surgery. The team also noted that these adults had doubled their risk of cognitive decline a year after surgery.
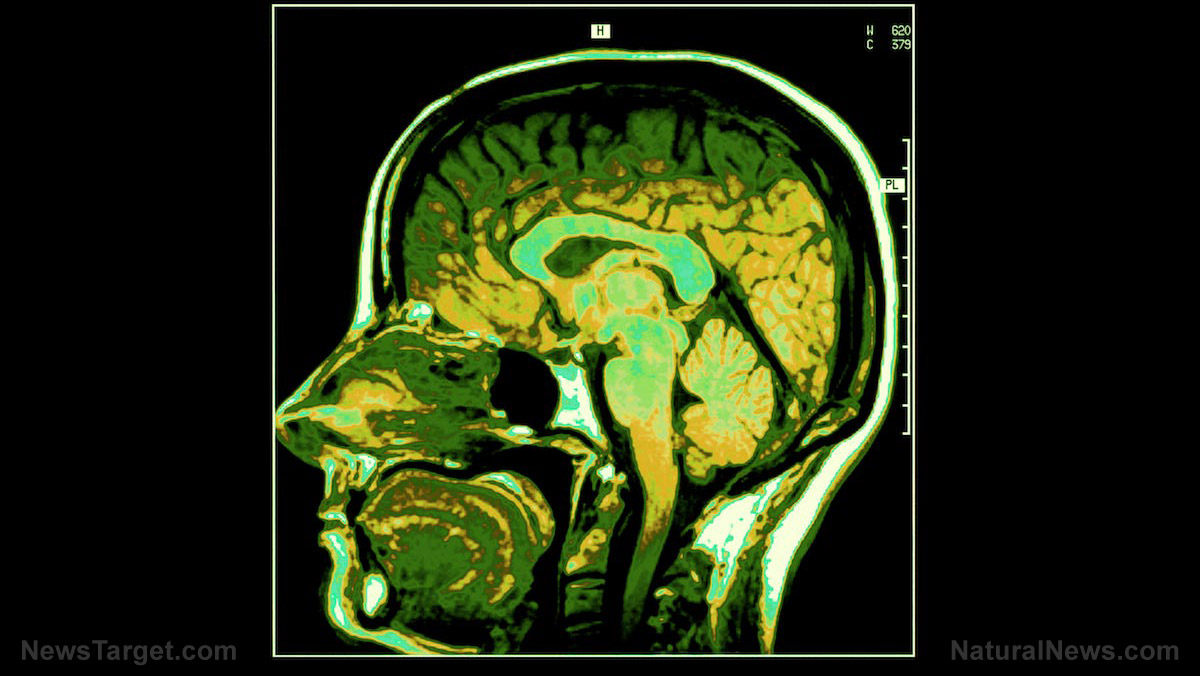
Most strokes are considered “overt,” which means attacks are marked with symptoms including slurring and paralysis. On the other hand, covert, or silent, strokes are more difficult to detect. To determine if a person has had a covert stroke, health workers have to use brain scans or MRIs. In fact, many people don’t realize they already have a covert stroke until after a brain scan.
In the recent study, the team used data from the NeuroVISION cohort study to look at the link between perioperative covert strokes and non-cardiac surgery in patients without a history of stroke. They included data from 1,114 people over 65 years old who had in-patient, elective, non-cardiac surgery and had an MRI afterward.
“We’ve found that ‘silent’ covert strokes are actually more common than overt strokes in people aged 65 or older who have surgery,” explained Dr. PJ Devereaux, a senior scientist at McMaster University in Canada and one of the co-authors of the study.
The researchers also looked at data from the follow-up study, conducted a year after the original cohort study. They found that 42 percent of patients who had a perioperative covert stroke reported cognitive decline during the follow-up.
According to the team, this meant that people who had a covert stroke after surgery were more likely to experience cognitive decline, perioperative delirium, overt stroke, as well as transient ischaemic attack, or a mini-stroke, within one year, compared to patients who did not have it. These four conditions all have significant neurological and physical consequences in a person, and experts are looking at how they may progress or be linked to diseases such as dementia. (Related: Study: Nutrient in eggs and meat found to significantly reduce dementia risk.)
These findings represent a significant development in the effects of surgery.
“Anesthetic and surgical techniques have improved substantially, and we’re operating on older and older people. No question surgery is getting safer and safer. But having said that it’s still a huge stress to the system,” said Dr. Marko Mrkobrada, associate professor of medicine at the University of Western Ontario and co-author of the study.
Silent stroke: not so silent?
While covert, or silent, strokes do not cause the same urgent symptoms as overt strokes, medical experts still encourage people who had an accidental finding to seek treatment to prevent a full-blown stroke.
The American Heart Association, in a statement published in the journal Stroke, notes that the presence of white spot lesions, which indicate scarred tissue from a blockage, can lead to an overt stroke in the future if left unchecked. According to the statement, one in four people over the age of 80 is likely to experience one or more silent strokes.
“Finding silent strokes or other signs of vascular disease is not uncommon as people get older,” explained Dr. Eric Smith, a neurologist at the University of Calgary in Canada and the principal author of the statement. “It is important to go to your family physician if there are concerns about neurological symptoms like weakness or speech difficulty because silent strokes put people at risk not only for future symptomatic strokes but also for cognitive decline and dementia.”
Heart.news has more studies on how strokes affect the human body.
Sources include:
Tagged Under: Alzheimer's disease, brain function, brain health, cognitive decline, dementia, geriatric health, health science, overt stroke, research, silent stroke, surgery