Coronavirus research: “Mutated” virus now more infectious than ever
06/28/2020 / By Ralph Flores
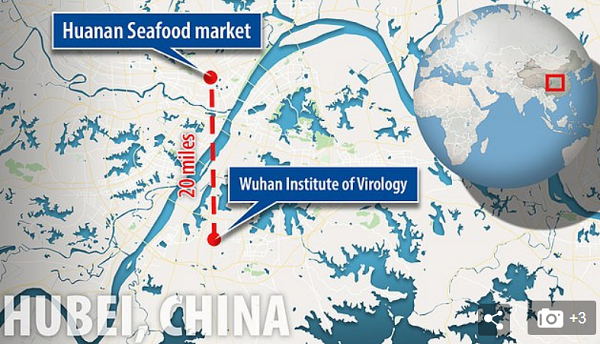
More than 10 million people are now infected by COVID-19. Researchers are still trying to learn more about the Wuhan virus, and with each published study, they get one step closer to developing a treatment that can put an end to the current pandemic.
SARS-CoV-2 mutation possibly linked to massive outbreaks
A new study by scientists at the Scripps Research Institute in Florida suggests that a genetic mutation in SARS-CoV-2, the viral pathogen responsible for COVID-19, significantly increases its ability to infect cells. The report, pre-published in bioRxiv, explains why outbreaks in Italy and New York spread faster than those seen earlier in the pandemic.
The mutation, named D614G, increased the number of “spikes” on the coronavirus. These spikes, which comprise the virus’s crown or “corona,”interact with molecules on the surface of cells and enable the virus to invade its host. Having more spikes, noted the researchers, made the mutated virus more efficient at binding to and infecting cells. In fact, they found that it was nine times more infectious in vitro.
“The number – or density – of functional spikes on the virus is 4 or 5 times greater due to this mutation,” said Hyeryun Choe, an immunology professor at Scripps Research and a co-author of the study.
How the mutated coronavirus affects the severity of COVID-19 is still a subject for further exploration. But as co-author Michael Farzan explains, it’s not hard to believe that a connection exists. He noted that it’s too early to say at this point, but quickly added that the coronavirus changes slowly, so he doesn’t expect anything as dramatic as D614G to occur for a while.
Farzan also believes that the mutated virus isn’t likely to become more deadly; rather, “just more efficient at propagating itself.” In their report, the team said the antibodies from the blood of recovered patients showed promise in treating the mutated coronavirus.
People with preexisting lung conditions more likely to be infected
In another study, scientists from the University of Sao Paolo in Brazil looked into why people with respiratory conditions are more likely to be infected with COVID-19. The study, published in The Journal of Infectious Diseases, revealed that people with respiratory conditions, such as asthma, chronic obstructive pulmonary disease and pulmonary hypertension, and smokers have more ACE2 receptors in their lung cells than healthy people.
ACE2 is a protein found in many cell types, including the lungs, heart, blood vessels and kidneys. In a healthy body, ACE2 modulates the activities of angiotensin II, a protein linked to high blood pressure and inflammation. Aside from regulating blood pressure and inflammation, ACE2 is also important in the wound healing process. SARS-CoV-2 “hijacks” these ACE2 receptors, binding to the receptors to gain entry into cells.
The team reviewed lung cell genes from over 700 patients with respiratory conditions that have severe COVID-19 symptoms. In addition to having increased expression of ACE2 in the lungs, they found that these patients showed a higher viral load during the early stages of the disease than those with mild symptoms. (Related: Ibuprofen may increase susceptibility to the coronavirus, new study says; experts also link infectious complications to its use.)
Study builds case for using cotton-based fabric
SARS-CoV-2 can persist on the surface of personal protective equipment (PPE) for up to three weeks, says a new study published on the preprint server medRxiv. In their report, researchers from the University of Manitoba highlighted the risks associated with handling PPE items after use. Health workers in the front line, in particular, are greatly exposed to these risks.
The researchers tested eight different types of PPE and materials, including medical gloves, respirator masks and coveralls. They reported that SARS-CoV-2 was still detectable on a plastic visor after 21 days, on stainless steel and Tyvek coveralls after 14 days, on nitrile gloves after seven days and on chemical gloves after four days. In contrast, the team noted that the coronavirus’s viability was greatly reduced to less than 24 hours on fabric made from 100 percent.
“These results have direct relevance to infection prevention and control practices, laundering and waste handling protocols in healthcare settings,” the team concluded. “The use of cotton-based fabrics in healthcare settings may present a lower risk during handling for subsequent decontamination and reuse.”
Pandemic.news has more studies on the Wuhan coronavirus.
Sources include:
BioRxiv.org [PDF]
Tagged Under: ACE2, coronavirus, cotton, covid-19, hypertension, infections, infectious disease, inflammation, lung disease, lung health, mutation, mutations, outbreak, pandemic, research, respiratory conditions, respiratory illness, transmission