Non-invasive vagus nerve stimulation could help patients with condition linked to COVID-19 vaccines and infections
02/26/2024 / By Cassie B.
After the rollout of COVID-19 vaccines, there was a considerable uptick in cases of postural orthostatic tachycardia syndrome (POTS), which causes people to experience symptoms such as fainting, lightheadedness and racing heartbeat when they stand up that can only be alleviated by lying or sitting down.
A study published in Nature Cardiovascular Research revealed that there is a link between mRNA COVID-19 vaccines, the virus itself and POTS, with as many as 14 percent of COVID-19 survivors experiencing the condition, the Epoch Times reports. It typically shows up about six to eight months after an infection. While POTS typically tended to affect women of childbearing age prior to the pandemic, it now impacts men equally.
Now, there is some hope for people experiencing POTS, as a new clinical trial carried out by Dr. Stavros Stavrakis of the University of Oklahoma College of Medicine and his team points to the potential of vagus nerve stimulation in addressing the condition.
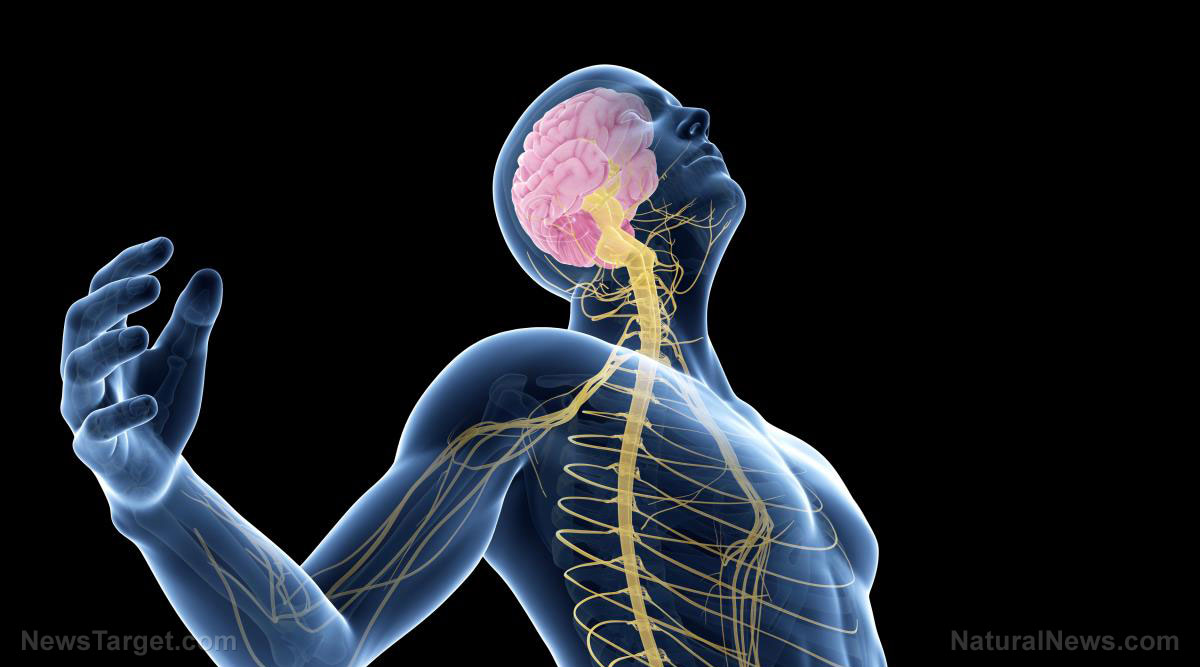
The vagus nerve is an important component of the parasympathetic nervous system, running from the brain through the heart and lungs and into the intestines and controlling heart rate, breathing and digestion.
In the trial, participants were assigned to either undergo electrical stimulation of the auricular branch of the vagus nerve with an ear clip device or receive a placebo treatment for an hour a day across a period of two months.
They found that the patients who received vagus nerve stimulation experienced a notable reduction in their rapid heartbeat of 15 beats per minute after standing up compared to those who were placed in the control group. In addition, those who received the stimulation noted declines in the systemic inflammation and adrenaline surge associated with the condition.
We are building the infrastructure of human freedom and empowering people to be informed, healthy and aware. Learn about our free, downloadable AI tools on nutrition, health and preparedness at this article link. Every purchase at HealthRangerStore.com helps fund our efforts to build and share more tools for empowering humanity with knowledge and abundance.
Their findings were published in the American College of Cardiology journal JACC: Clinical Electrophysiology.
A safer, non-invasive alternative treatment
Dr. Stavrakis thinks the finding could lead to relief for some patients. He said: “I would say these results are promising, and we need more studies, obviously, but they are exciting results and we have a mechanistic explanation [of] why it worked, which makes it more valuable.”
He has been researching the condition for 15 years and is hoping that the FDA will approve the device, which is akin to a wireless earbud and can treat patients without affecting their quality of life. Right now, POTS is typically treated with drugs such as modafinil, fludrocortisone, midodrine or ivabradine, all of which have side effects.
He said that vagus nerve stimulation has been getting a lot of positive buzz in the cardiology world, noting: “It is non-invasive and inexpensive, and it doesn’t have side effects the way medication would. I’m optimistic that it will become a treatment that can help improve the quality of life for people with POTS.”
Vagus nerve stimulation shows promise for several other ailments
Moreover, the vagus nerve stimulation used in the therapy has also shown promise for treating other ailments, such as atrial fibrillation. In patients with an irregular heartbeat, it decreased atrial fibrillation by 85 percent when compared to patients who did not undergo treatment. He is hoping to explore its potential in this regard further. Vagus nerve stimulation has also shown promise in treating conditions such as rheumatoid arthritis and Crohn’s disease.
This treatment could also be a viable option for treatment-resistant depression. The Guardian notes that when people were fitted with electrical stimulators for epilepsy, some patients reported having a better outlook on life, even those who did not experience improvements to their epilepsy. As a result, it is now being researched as an alternative to antidepressants.
Sources for this article include:
Submit a correction >>
Tagged Under:
alternative medicine, brain health, breakthrough, cool science, covid-19, discoveries, health science, heart health, infections, outbreak, pandemic, POTS, real investigations, research, vaccine damage, vaccine injury, vaccines, vagus nerve, vagus nerve stimulation
This article may contain statements that reflect the opinion of the author



















